Recently, I read an opinion titled When I Became A Mother, Feminism Let Me Down. The gist of it was that some (not all!) feminists, while empowering women and girls to be anything they want to be and to do anything a man or a boy does, they fail in uplifting the motherhood aspect of a woman’s life, should she choose to become a mother. In other words, even (or especially, in some cases) feminists look down on the women who chose to switch from a paid job and professional career to an unpaid stay-at-home mom career, as if being a mother is somehow beneath what a woman can be and can achieve. As if raising the next generation of humans to be rational, informed, well-behaved social actors instead of ignorant brutal egomaniacs is a trifling matter, not to be compared with the responsibilities and struggles of a CEO position.
Patriarchy notwithstanding, a woman can do anything a man can. And more. The ‘more’ refers to, naturally, motherhood. Evidently, fatherhood is also a thing. But the changes that happen in a mother’s brain and body during pregnancy, breastfeeding, and postpartum periods are significantly more profound than whatever happens to the most loving and caring and involved father.
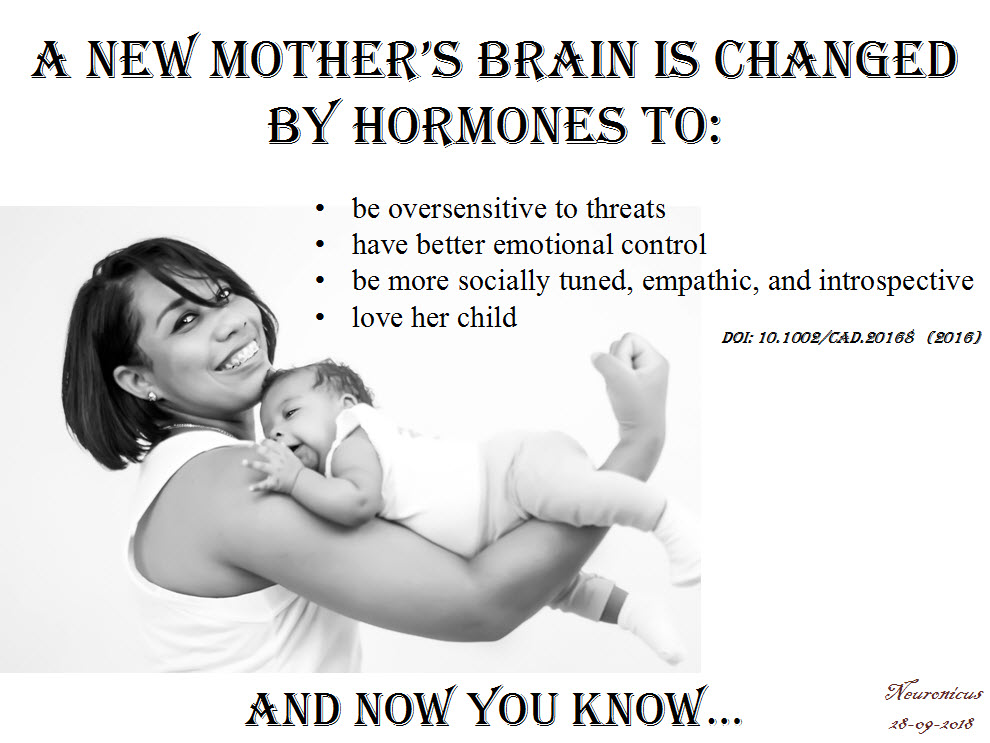
Kim (2016) bundled some of these changes in a nice review, showing how these drastic and dramatic alterations actually have an adaptive function, preparing the mother for parenting. Equally important, some of the brain plasticity is permanent. The body might spring back into shape if the mother is young or puts into it a devilishly large amount of effort, but some brain changes are there to stay. Not all, though.
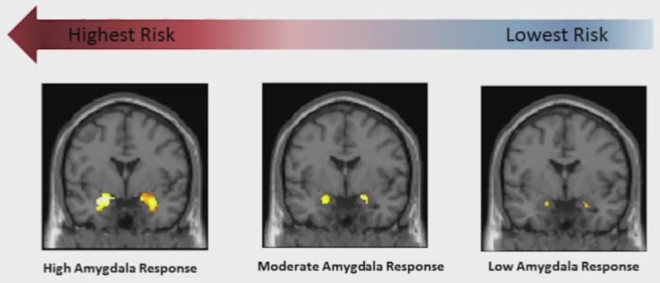
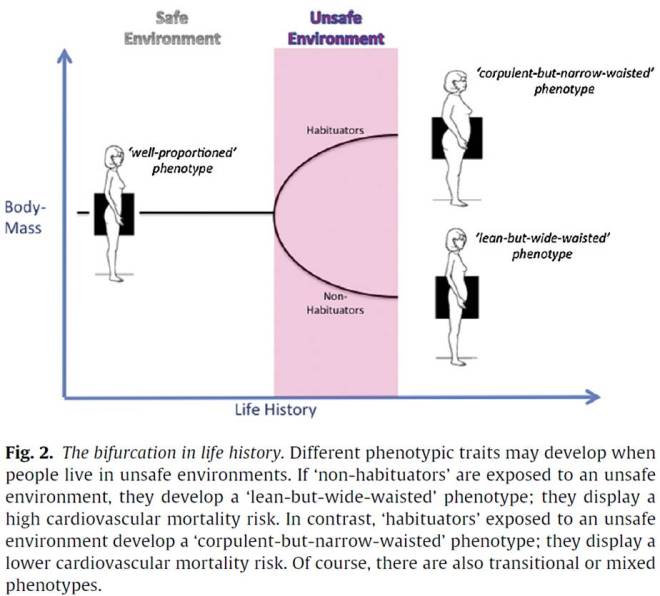
One of the most pervasive findings in motherhood studies is that hormones whose production is increased during pregnancy and postpartum, like oxytocin and dopamine, sensitize the fear circuit in the brain. During the second trimester of pregnancy and particularly during the third, expectant mothers start to be hypervigilent and hypersensitive to threats and to angry faces. A higher anxiety state is characterized, among other things, by preferentially scanning for threats and other bad stuff. Threats mean anything from the improbable tiger to the 1 in a million chance for the baby to be dropped by grandma to the slightly warmer forehead or the weirdly colored poopy diaper. The sensitization of the fear circuit, out of which the amygdala is an essential part, is adaptive because it makes the mother more likely to not miss or ignore her baby’s cry, thus attending to his or her needs. Also, attention to potential threats is conducive to a better protection of the helpless infant from real dangers. This hypersensitivity usually lasts 6 to 12 months after childbirth, but it can last lifetime in females already predisposed to anxiety or exposed to more stressful events than average.
Many new mothers worry if they will be able to love their child as they don’t feel this all-consuming love other women rave about pre- or during pregnancy. Rest assured ladies, nature has your back. And your baby’s. Because as soon as you give birth, dopamine and oxytocin flood the body and the brain and in so doing they modify the reward motivational circuit, making new mothers literally obsessed with their newborn. The method of giving birth is inconsequential, as no differences in attachment have been noted (this is from a different study). Do not mess with mother’s love! It’s hardwired.
Another change happens to the brain structures underlying social information processing, like the insula or fusiform gyrus, making mothers more adept at self-motoring, reflection, and empathy. Which is a rapid transformation, without which a mother may be less accurate in understanding the needs, mental state, and social cues of the very undeveloped ball of snot and barf that is the human infant (I said that affectionately, I promise).
In order to deal with all these internal changes and the external pressures of being a new mom the brain has to put up some coping mechanisms. (Did you know, non-parents, that for the first months of their newborn lives, the mothers who breastfeed must do so at least every 4 hours? Can you imagine how berserk with sleep deprivation you would be after 4 months without a single night of full sleep but only catnaps?). Some would be surprised to find out – not mothers, though, I’m sure – that “new mothers exhibit enhanced neural activation in the emotion regulation circuit including the anterior cingulate cortex, and the medial and lateral prefrontal cortex” (p. 50). Which means that new moms are actually better at controlling their emotions, particularly at regulating negative emotional reactions. Shocking, eh?
Finally, it appears that very few parts of the brain are spared from this overhaul as the entire brain of the mother is first reduced in size and then it grows back, reorganized. Yeah, isn’t that weird? During pregnancy the brain shrinks, being at its lowest during childbirth and then starts to grow again, reaching its pre-pregnancy size 6 months after childbirth! And when it’s back, it’s different. The brain parts heavily involved in parenting, like the amygdala involved in the anxiety, the insula and superior temporal gyrus involved in social information processing and the anterior cingulate gyrus involved in emotional regulation, all these show increased gray matter volume. And many other brain structures that I didn’t list. One brain structure is rarely involved only in one thing so the question is (well, one of them) what else is changed about the mothers, in addition to their increased ability to parent?
I need to add a note here: the changes that Kim (2016) talks about are averaged. That means some women get changed more, some less. There is variability in plasticity, which should be a pleonasm. There is also variability in the human population, as any mother attending a school parents’ night-out can attest. Some mothers are paranoid with fear and overprotective, others are more laissez faire when it comes to eating from the floor.
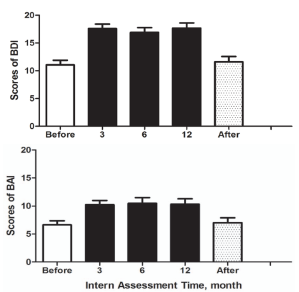
But SOME changes do occur in all mothers’ brains and bodies. For example, all new mothers exhibit a heightened attention to threats and subsequent raised levels of anxiety. But when does heightened attention to threats become debilitating anxiety? Thanks to more understanding and tolerance about these changes, more and more women feel more comfortable reporting negative feelings after childbirth so that now we know that postpartum depression, which happens to 60 – 80% of mothers, is a serious matter. A serious matter that needs serious attention from both professionals and the immediate social circle of the mother, both for her sake as well as her infant’s. Don’t get me wrong, we – both males and females – still have a long way ahead of us to scientifically understand and to socially accept the mother brain, but these studies are a great start. They acknowledge what all mothers know: that they are different after childbirth than the way they were before. Now we have to figure out how are they different and what can we do to make everyone’s lives better.
Kim (2016) is an OK review, a real easy read, I recommend it to the non-specialists wholeheartedly; you just have to skip the name of the brain parts and the rest is pretty clear. It is also a very short review, which will help with reader fatigue. The caveat of that is that it doesn’t include a whole lotta studies, nor does it go in detail on the implications of what the handful cited have found, but you’ll get the gist of it. There is a vastly more thorough literature if one would include animal studies that the author, curiously, did not include. I know that a mouse is not a chimp is not a human, but all three of us are mammals, and social mammals at that. Surely, there is enough biological overlap so extrapolations are warranted, even if partially. Nevertheless, it’s a good start for those who want to know a bit about the changes motherhood does to the brain, behavior, thoughts, and feelings.
Corroborated with what I already know about the neuroscience of maternity, my favourite takeaway is this: new moms are not crazy. They can’t help most of these changes. It’s biology, you see. So go easy on new moms. Moms, also go easy on yourselves and know that, whether they want to share or not, the other moms probably go through the same stuff. The other moms are doing better than you are either. You’re not alone. And if that overactive threat circuit gives you problems, i.e. you feel overwhelmed, it’s OK to ask for help. And if you don’t get it, ask for it again and again until you do. That takes courage, that’s empowerment.
P. S. The paper doesn’t look like it’s peer-reviewed. Yes, I know the peer-reviewing publication system is flawed, I’ve been on the receiving end of it myself, but it’s been drilled into my skull that it’s important, flawed as it is, so I thought to mention it.
REFERENCE: Kim, P. (Sept. 2016). Human Maternal Brain Plasticity: Adaptation to Parenting, New Directions for Child and Adolescent Development, (153): 47–58. PMCID: PMC5667351, doi: 10.1002/cad.20168. ARTICLE | FREE FULLTEXT PDF
By Neuronicus, 28 September 2018



 Last year a new peer-reviewed journal called Neurobiology of Stress made its debut. The journal is published by Elsevier, who, in an uncharacteristic move, has provided Open Access for its first three issues. So hurry up and download the papers.
Last year a new peer-reviewed journal called Neurobiology of Stress made its debut. The journal is published by Elsevier, who, in an uncharacteristic move, has provided Open Access for its first three issues. So hurry up and download the papers.