Among the many humorous sayings, puns, and jokes that one inevitably encounters on any social medium account, one that was popular this year was about the similarity between putting a 2 year old to bed and putting your drunk friend to bed, which went like this: they both sing to themselves, request water, mumble and blabber incoherently, do some weird yoga posses, cry, hiccup, and then they pass out. The joke manages to steal a smile only if someone has been through both situations, otherwise it looses its appeal.
Being exposed to both situations, I thought that while the water request from the drunk friend is a response to the dehydrating effects of alcohol, the water request from the toddler is probably nothing more than a delaying tactic to postpone bedtime. Whether there may or may not be some truth to my assumption in the case of the toddler, here is a paper to show that there is definitely more to the water request than meets the eye.
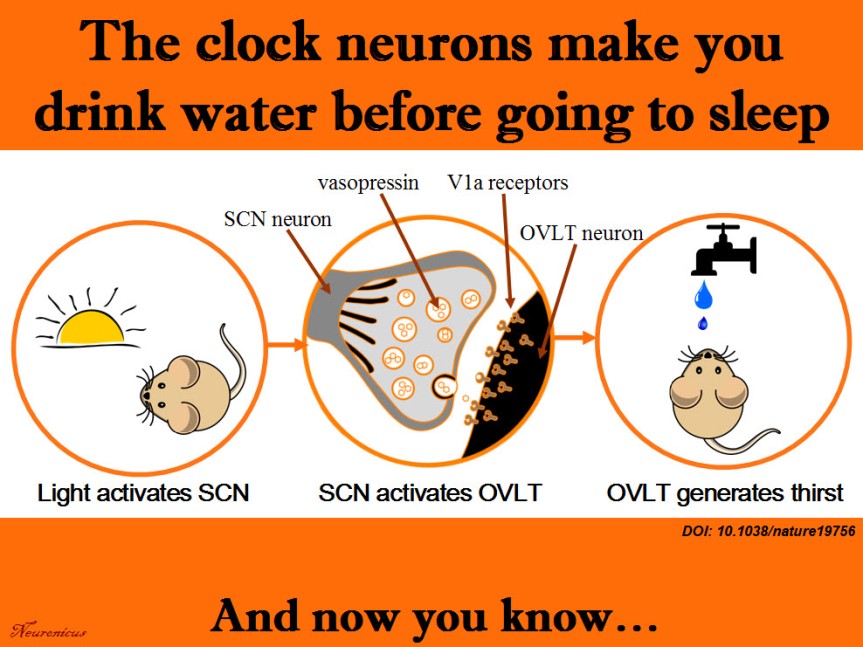
Generally, thirst is generated by the hypothalamus when its neurons and neurons from organum vasculosum lamina terminalis (OVLT) in the brainstem sense that the blood is either too viscous (hypovolaemia) or too salty (hyperosmolality), both phenomena indicating a need for water. Ingesting water would bring these indices to homeostatic values.
More than a decade ago, researchers observed that rodents get a good gulp of water just before going to sleep. This surge was not motivated by thirst because the mice were not feverish, were not hungry and they did not have a too viscous or a too salty blood. So why do it then? If the rodents are restricted from drinking the water they get dehydrated, so obviously the behavior has function. But is not motivated by thirst, at least not the way we know it. Huh… The authors call this “anticipatory thirst”, because it keeps the animal from becoming dehydrated later on.
Since the behavior occurs with regularity, maybe the neurons that control circadian rhythms have something to do with it. So Gizowski et al. (2016) took a closer look at the activity of clock neurons from the suprachiasmatic nucleus (SCN), a well known hypothalamic nucleus heavily involved in circadian rhythms. The authors did a lot of work on SCN and OVLT neurons: fluorescent labeling, c-fos expression, anatomical tracing, optogenetics, genetic knockouts, pharmacological manipulations, electrophysiological recordings, and behavioral experiments. All these to come to this conclusion:
SCN neurons release vasopressin and that excites the OVLT neurons via V1a receptors. This is necessary and sufficient to make the animal drink the water, even if it’s not thirsty.
That’s a lot of techniques used in a lot of experiments for only three authors. Ten years ago, you needed only one, maybe two techniques to prove the same point. Either there have been a lot of students and technicians who did not get credit (there isn’t even an Acknowledgements section. EDIT: yes, there is, see the comments below or, if they’re missing, the P.S.) or these three authors are experts in all these techniques. In this day and age, I wouldn’t be surprised by either option. No wonder small universities have difficulty publishing in Big Name journals; they don’t have the resources to compete. And without publishing, no tenure… And without tenure, less research… And thus shall the gap widen.
Musings about workload aside, this is a great paper, shedding light on yet another mysterious behavior and elucidating the mechanism behind it. There’s still work to be done though, like answering how accurate is the SCN in predicting bedtime to activate the drinking behavior. Does it take its cues from light only? Does ambient temperature play a role and so on. This line of work can help people that work in shifts to prevent certain health problems. Their SCN is out of rhythm and that can influence deleteriously the activity of a whole slew of organs.
Reference: Gizowski C, Zaelzer C, & Bourque CW (28 Sep 2016). Clock-driven vasopressin neurotransmission mediates anticipatory thirst prior to sleep. Nature, 537(7622): 685-688. PMID: 27680940. DOI: 10.1038/nature19756. ARTICLE
By Neuronicus, 5 October 2016
EDIT (12 Oct 2016): P.S. The blog comments are automatically deleted after a period of time. In case of this post that would be a pity because I have been fortunate to receive comments from at least one of the authors of the paper, the PI, Dr. Charles Bourque and, presumably under pseudonym, but I don’t know that for sure, also the first author, Claire Gizowski. So I will include here, in a post scriptum, the main idea of their comments. Here is an excerpt from Dr. Bourque’s comment:
“Let me state for the record that Claire accomplished pretty much ALL of the work in this paper (there is a description of who did what at the end of the paper). More importantly, there were no “unthanked” undergraduates, volunteers or other parties that contributed to this work.”
My hat, Ms. Gizowski. It is tipped. To you. Congratulations! With such an impressive work I am sure I will hear about you again and that pretty soon I will blog about Dr. Gizowski.


